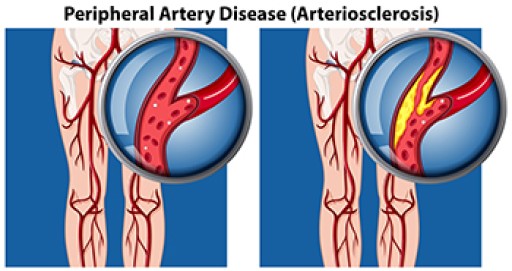
Peripheral artery disease, or PAD, which reduces blood flow to the feet due to narrowed arteries, is often caused by fatty deposits known as atherosclerosis. When circulation to the lower limbs is restricted, people may experience cold feet, skin color changes, slow-healing wounds, or painful cramping while walking. Over time, symptoms of peripheral artery disease can progress and may lead to serious complications, including ulcers or tissue damage. Hair loss on the feet and slow-growing toenails are other indications of poor circulation. People with diabetes, high blood pressure, or a history of smoking are at a higher risk of developing PAD. A podiatrist may detect reduced pulses, temperature differences, or other signs during a foot exam and can recommend diagnostic testing, such as an ankle-brachial index. If PAD is identified early, a podiatrist may suggest medical treatment, and, in severe cases, surgery to restore blood flow and prevent further damage. If you are experiencing symptoms of peripheral artery disease, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment options.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Associates in Podiatry, PC. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Pittsburgh-South Hills, and Pittsburgh-Bellevue, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.